Overview
A common treatment for fibrolamellar carcinoma (FLC) is surgical removal (resection) of the tumor. Doctors sometimes use the term resectable to describe cancers they believe can be removed by surgery and unresectable to describe those they think are too difficult to be entirely removed by surgery. Surgical treatments for FLC include both curative surgery and palliative surgery. Curative surgery removes all visible traces of cancer from the body. Palliative surgery means the goal is to “debulk” the tumor, improve symptoms, lessen pain or provide better quality of life, even when all visible tumor can’t be removed.
Surgery is the only treatment for FLC that is proven to be potentially curative. As a result, many patients will go to great lengths to make sure surgery is a viable option for their treatment, including:
- consulting with multiple surgeons about whether or not their disease can be completely resected
- working with their surgical and oncology teams to identify systemic treatments or interventional radiology treatments that could potentially shrink the disease enough to make them a candidate for surgery.
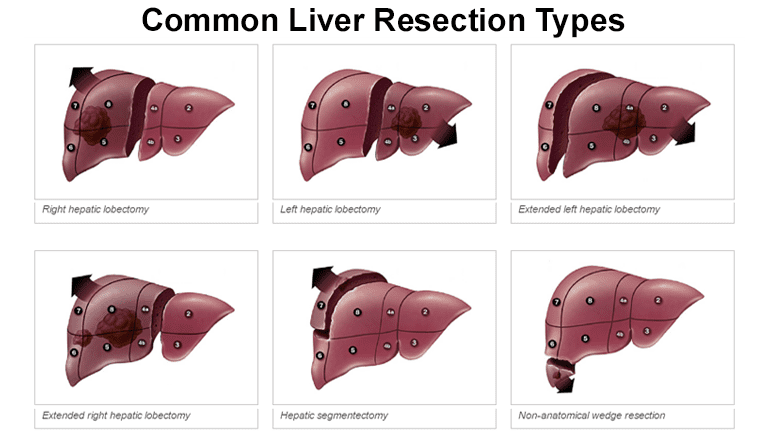
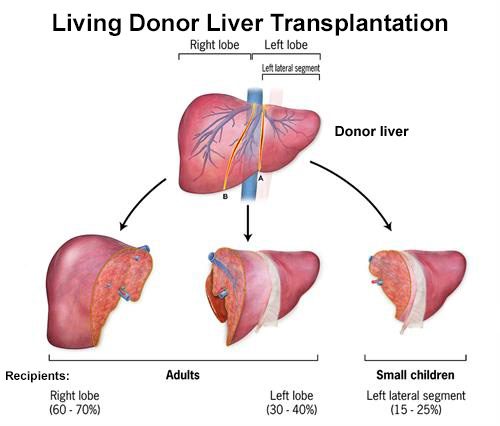
Because the liver is the only organ which can regenerate itself, it can grow to compensate for the removed portions after surgery. This can allow surgeons to resect up to 70-80% of the liver in exceptional cases. After liver surgery, liver function typically returns to normal within 2 to 3 weeks of resection surgery and liver size returns to normal within 3 to 6 months.
Surgical approaches for FLC
Two main types of surgery are used to treat FLC that has not spread beyond the liver. These include:
Tumor recurrence
It is possible for tumors to recur (return) even when resection and/or transplantation has been considered successful. Different studies have shown that between 43 percent and 65 percent of all patients with liver tumors (including, but not exclusive to those with fibrolamellar) have recurrences within two years of a liver resection.
For that reason, patients are typically monitored with regular checkups and CT and/or MRI scans at regular intervals to watch for signs of recurrence. Most recurring tumors tend to appear within a few years of surgery, but patients are typically monitored for 10 years or more to be on the safe side. Depending on where they show up, recurring tumors are frequently treated with another surgery.
Please note: The Fibrolamellar Cancer Foundation does not provide medical advice or recommend any specific organizations or services. We provide website users with information to help them better understand their health conditions and current approaches to the diagnosis and treatment of FLC. Always seek the advice of your physician or other qualified healthcare providers.