A perspective on Rare Cancer Day.
This year more than 600,000 lives in the US will be lost to cancer. The five most common malignancies account for half of these deaths. Most of the victims are elderly; fewer than 2% of cancer fatalities occur under age 40. Rarer cancers, especially those affecting youthful patients, receive far less attention and research funding than more prevalent forms of this disease. Why, then, does the Fibrolamellar Cancer Foundation (FCF) focus its efforts on research into an ultra-rare liver cancer of adolescents and young adults?
Each patient and caregiver attending FCF’s Patient & Family Gathering in Vermont earlier this month provided a compelling reason to fight against fibrolamellar carcinoma (FLC). These are extraordinary individuals – brave and resourceful in the face of a shockingly unexpected, relentless illness. They urgently need better treatments for the disease. However, beyond compassion, other reasons have helped persuade a group of outstanding physicians and scientists to focus their efforts on FLC. Chief among them is the fact that many breakthroughs in our understanding of cancer and in the development of effective therapies have flowed from research on rare cancers like FLC. Examples include:
- Chemical carcinogens were first identified thanks to a physician’s observation that young chimney sweeps exposed to soot trapped in their clothing developed a characteristic scrotal cancer (1770s)
- Cancer chemotherapy advanced through the development of successful treatments for pediatric leukemia and other rare childhood cancers (1945-1970s)
- Monoclonal antibody anti-cancer medicines were first developed to treat rare lymphomas (Rituxan®, FDA-approved 1997) and a genetically distinct subset (10-20%) of breast cancers (Herceptin®, 1998)
- Drug therapy targeting an “oncoprotein,” a specific aberrant protein that drives a cancer’s growth, was first introduced to treat the rare cancer chronic myeloid leukemia (CML) (Gleevec®, 2001)
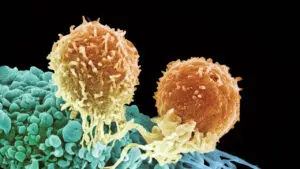
- CAR (chimeric antigen receptor) T-cell therapy was first used to treat a rare pediatric leukemia (Kymriah®, 2017).
What are the advantages of researching rare cancers? While all cancers share fundamental hallmarks, it is a remarkably heterogeneous disease. Cancer arises because of genetic events – the activation of cancer driver genes (“oncogenes”) coupled with the loss of “tumor suppressors.” These mutations cause cells to proliferate and spread. In common cancers, the critical mutated genes frequently differ from patient to patient. Moreover, many of the most prevalent cancers are genetically unstable, enabling drug resistant cells, sometimes with new driver mutations, to emerge as patients receive therapy. By contrast, most rare cancers are genetically simpler, more homogeneous, and more stable than common ones. This makes rare cancers more straightforward to tackle.
FLC results from a genetic mutation which converts protein kinase A (PKA), an important enzyme involved in regulating cell growth and metabolism, into a cancer driver. Almost always, the mutation fuses two adjacent genes (DNAJB1::PRKACA) in the tumor cells, leading to the production of a “chimeric” protein (abbreviated “DP”), in which a segment from an unrelated protein replaces a small piece of the normal PKA protein chain.
The most compelling precedent for a cancer drug targeting a driver protein remains Gleevec, developed to treat the rare leukemia CML. Like FLC, CML results from the activation of a protein kinase (in this case one named ABL) via a gene fusion. Gleevec selectively inhibits the ABL kinase. This drug proved a lifesaver. Before its discovery, CML was almost always fatal. Today, the great majority of patients with CML live out a normal lifespan. The pioneering team that introduced the novel therapeutic approach of blocking activated protein kinases chose to focus on CML, rather than a common cancer, because every case was associated with an ABL gene fusion. At the time, no other human cancer had been identified in which a single oncogenic driver was universally implicated.
Unfortunately for FLC patients, the inhibitors of the DP driver protein developed to date also inactivate normal PKA, which is needed to regulate the heartbeat and other functions essential for life. However, FLC investigators are developing new ways to attack DP-driven cancer cells by harnessing the immune system and by inhibiting specific downstream processes driven by the DP kinase. Many of these approaches represent novel ways to attack a cancer. Already, the “therapeutic vaccine” efforts underway in the U.S. and Germany are showing exceptionally promising early results. Each of these successes help reinforce strategies which could potentially apply to many other cancers.
As history has shown, research on a rare, often neglected “little child” among cancers can strongly impact broader efforts to tame this beastly disease. On this Rare Cancer Day, we should all remember that research into specific rare cancers, like fibrolamellar carcinoma, can ultimately improve the prospects of those grappling with many different varieties of the disease.