Overview
Targeted therapy is a newer type of cancer treatment that uses drugs or other substances to more precisely identify and attack certain types of cancer cells. Targeted drugs block the growth and spread of cancer by interfering with specific biochemical pathways in tumor cells that are important to their growth or survival. By targeting specific molecules involved in those pathways, the drugs can inhibit the growth of the tumor while limiting damage to normal cells. Targeted therapy is sometimes called “molecular targeted therapy” or “precision medicine”.
Targeted therapies differ from traditional chemotherapy in that targeted therapies try to alter how the cancer cells work. To do that, they focus on part of the cancer cell that makes it different from a healthy cell. In contrast, most standard chemotherapies kill rapidly dividing cancerous and normal cells. Like chemotherapy, targeted therapy drugs enter the bloodstream and reach most areas of the body, which makes them potentially useful against cancers that have spread. Because standard chemo is not very effective in most patients with liver cancer, doctors are focusing more on using targeted therapies.
Types of targeted therapy
There are many different types of targeted cancer drugs. They include both
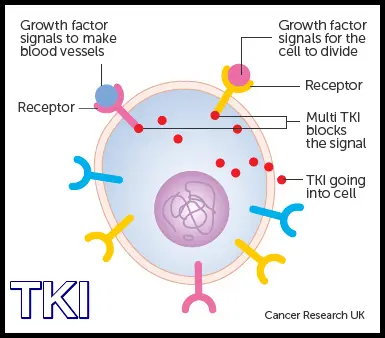
- small molecule drugs that are are small enough to enter a cancer cell and target a specific substance inside the cell, and
- large molecule drugs that can’t fit inside a cell, but work by weakening or destroying proteins or enzymes on the cancer cell’s surface.
Most of these targeted therapy drugs work by one of the following mechanisms:
- Slowing or stopping the development of new blood vessels that feed the cancer cell (This type of drug is called an angiogenesis inhibitor)
- Blocking signals that tell a cancer cell to grow or divide
- Triggering the immune system to attack the cancer cell
- Changing specific proteins within a cancer cell, so the cell dies
- Carrying other types of treatments (like chemotherapy) directly to a cancer cell to kill it, while leaving normal cells alone (These are often called antibody-drug conjugates or ADCs).
Targeted therapies used in liver cancer and FLC
FLC patients are often treated with the following targeted therapies. All are approved treatments for HCC:
Rationale for combination therapies
As with any systemic therapy, cancer cells can become resistant to targeted therapy drugs, causing the drugs to become ineffective over time. This resistance can occur if the tumor cells mutate so the drug no longer interacts well with the cell targets, or if the tumor finds a new pathway to grow that does not depend on the drug’s target. To help avoid this problem, targeted therapies are frequently delivered in combination with other drugs, rather than alone.

For many cancers like fibrolamellar, it is believed that combinations of drugs – a “one-two punch” of treatment – can achieve many benefits. Potential benefits include:
- Reducing tumor resistance to the treatment. By using drug combinations, the risk that a tumor is resistant to the drug decreases.
- Attacking multiple targets at once. The use of drug combinations allows doctors to target several factors driving a cancer’s growth simultaneously. Theoretically, working on multiple molecular targets at the same time should raise the chances of killing cancer cells and eliminating a tumor.
- Taking advantage of drug synergies. Sometimes a combination of drugs can be synergistic, meaning the impact of the combination is bigger than sum of the individual effects of each drug. For example, one drug could sensitize a tumor cell to another drug, making the combination much more effective than either drug alone.
However, combination therapies also have some risks or disadvantages, including:
- Increased side effects could be experienced because more than one drug is used
- The drugs could potentially interact in ways that cause additional new side effects.
Because patients with fibrolamellar carcinoma tend to be young and (aside from the cancer) usually have no underlying liver disease, many believe the benefits of drug combinations outweigh their risks. Consequently, there is a lot of activity, from early research to clinical trials, focused on investigating the use of different combination therapies in liver cancer and FLC.
Role of genomic profiling tests
Genomic profiling provides information about the specific genetic makeup of an individual patient’s cancer cells. To get this information, a sample of tumor tissue from a recent surgery or biopsy is analyzed to identify changes in the DNA (and sometimes the RNA) of the cancer cells. These tests generally do not perform a complete genomic analysis of the patient’s tissue. Instead they often look for specific mutations for which a drug treatment is already available, or under development.
For some patients, an “actionable target” is found. This means that the test discovered a particular mutation in a patient’s tumor that can be attacked by an existing drug.
Unlike many other cancers, FLC tumors tend to have few genetic mutations other than the DNAJB1–PRKACA fusion gene. As a result, many FLC patients do not receive actionable results from these tests. Nevertheless, many FLC patients opt to pursue the testing, hoping to find and potentially benefit from new emerging targeted cancer treatments.
Many major medical centers offer this type of testing to their patients. In addition, many commercial laboratories (including Caris, Foundation Medicine, Guardant, Molecular Health, and Paradigm) also offer tumor profiling tests. If interested, patients should speak with their medical teams about the costs and potential benefits of genomic or molecular testing.
Please note: The Fibrolamellar Cancer Foundation does not provide medical advice or recommend any specific organizations or services. We provide website users with information to help them better understand their health conditions and current approaches to the diagnosis and treatment of FLC. Always seek the advice of your physician or other qualified healthcare providers.