Overview
Chemotherapy – the use of powerful drugs to kill dividing cancer cells and prevent them from growing – is commonly used in treating fibrolamellar. Because it is a systemic treatment, chemotherapy can reach cells almost anywhere in the body. Most chemotherapies are cytotoxic chemicals, meaning that they kill cells. Chemotherapy is used as a treatment because rapidly growing and dividing cancer cells are generally more susceptible to damage by the chemo agents than normal cells.
Chemotherapy is used in three ways:
- to kill or shrink tumors when surgery is not possible, sometimes in the hope of enabling surgery after sufficient tumor shrinkage
- to kill cancer cells that have spread beyond the liver, or
- as an adjuvant therapy in combination with surgery and/or radiation
- to enhance the response of a tumor to radiation therapy
- to destroy residual cancer cells that could be left behind after surgery.
Chemotherapies used in liver cancer and FLC
There are many chemotherapy drugs that doctors can choose from. Oncologists generally choose which drug to use based on a standard protocol for a disease (the drugs with the history of the best outcomes), the stage of the cancer, as well as the health and age of the patient. Because of the rarity of cases of FLC and the lack of systematic studies to establish a clear “standard of care”, many oncologists prescribe chemotherapies for FLC based on treatments that have been shown to be effective in HCC, plus their best judgement. In light of the limited evidence supporting the use of any particular treatment in FLC, a wide variety of treatments are currently prescribed.
Because FLC tumors can be resistant to many chemotherapy drugs, oncologists often use a combination of 2 or 3 of these drugs to achieve the best results. (See rationale for combination therapies in the targeted therapy section.) The response rate to chemotherapy drugs with FLC is roughly 25 percent.1
Chemotherapies that are used to treat fibrolamellar patients include:
- 5-fluorouracil (5-FU)
- Capecitabine (Xeloda) – Capecitabine is closely related to 5-FU. Instead of being an infused drug, capecitabine comes in a pill form. It is metabolized by the body into 5-FU.
- 5-FU plus interferon
- FOLFOX (5-FU, oxaliplatin and leucovorin)
- Gemcitabine (Gemzar)
- GEMOX (gemcitabine plus oxaliplatin)
- Oxaliplatin (Eloxatin)
- Doxorubicin (pegylated liposomal doxorubicin)
- Cisplatin
- Mitoxantrone (Novantrone).
Chemotherapy administration
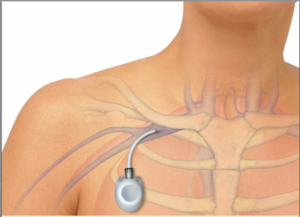
Chemotherapy is often administered by injection or infusion, though some can be administered in pill or capsule form, which can be taken at home. Since many chemotherapies are strong medications, they can potentially cause damage if repeatedly injected into a peripheral vein in a patient’s arm. Consequently, doctors will often insert a port, a nickel-sized device with an attached catheter (tube) that ends close to the heart. This position allows infused agents to be spread throughout the body quickly and efficiently, and the port allows medication to be injected into it rather than through frequent needle stick injections. The port is usually implanted under the skin in a patient’s upper chest, and can remain in place as long as necessary. Insertion of the port is done in an operating room using local anesthesia while the patient is sedated, but awake.
Doctors give chemotherapy in cycles, with each period of treatment followed by a rest period to give the body time to recover. The treatment schedule varies with the patient and the drugs used.
Other methods of administering chemotherapy that are sometimes used in FLC include:
- Transarterial chemoembolization (TACE) – with TACE, a catheter is inserted in the groin and guided into the artery that supplies the cancerous tumor. Chemotherapy drugs are delivered straight to that artery, with the goal of disrupting the tumor’s blood supply while trapping the chemotherapy inside the tumor. (See the interventional radiology section for more information)
- Percutaneous hepatic perfusion (PHP) – In PHP, the liver’s blood supply is temporarily disconnected from the body’s circulation and chemotherapy drugs are circulated through the liver for a short time. Unlike traditional chemotherapy, in which medications circulate throughout the entire body, PHP targets the liver only. As a result, oncologists can treat tumors with higher doses of chemotherapy using PHP than are possible when the chemo is given systemically.
Both TACE and PHP are minimally invasive surgeries that can be used in conjunction with other treatments, such as surgery, radiation or ablation.
Side Effects
Everyone reacts to chemotherapy drugs differently, but many side effects are common. Most chemotherapy drugs work by attacking cells in your body that are dividing quickly. Cancer cells form new cells more rapidly than normal cells. However, other cells in your body also divide quickly, like those in the bone marrow, the lining of the mouth and intestines, and hair follicles. As a result, these cells can also be affected by the chemotherapy drugs, which can lead to side effects. While the exact side effects of chemotherapy depend on the specific drug, dosage and length of time they are taken, typical side effects include:
- hair loss
- nausea
- diarrhea
- infertility
- extreme fatigue (due to low red blood cell counts)
- increased risk of infection (due to low white blood cell counts)
- neuropathy (tingling, burning or numbness, most often in the fingers and feet).
While all of these side effects are unpleasant, not all are serious. Talking to the treatment team about them is important, as adjustments can sometimes be made when a side effect is particularly debilitating.
1https://emedicine.medscape.com/article/278354-treatment
Please note: The Fibrolamellar Cancer Foundation does not provide medical advice or recommend any specific organizations or services. We provide website users with information to help them better understand their health conditions and current approaches to the diagnosis and treatment of FLC. Always seek the advice of your physician or other qualified healthcare providers.
