This spring, based on a study partially funded by FCF, a six-institution team led by Paul Thomas (St. Jude Children’s Research Hospital) and Scott Strome (University of Tennessee) published an article in Cell Reports Medicine about the isolation of T-cell receptors specific for the fusion protein driver of fibrolamellar carcinoma (FLC). (Click here to read the publication). Below is a discussion of the implications of that study and other recent research efforts on future FLC immunotherapy treatments as summarized by Mark Furth, Chief Science Officer of FCF.
Background
Therapies that enhance the body’s immune response against tumor cells are dramatically improving outcomes for patients with many cancers. Immunotherapy harnesses the ability of certain white blood cells to hunt down and destroy cancer cells. For such search and destroy missions, “killer T cells” (a type of lymphocyte) recognize specific chemical features, called antigens, that mark abnormal cells. To do so, each killer T cell produces on its surface a receptor protein (called a T-cell receptor or TCR) that binds specifically to a unique antigen, like a key matches a lock. These TCRs recognize peptides, which are fragments of proteins from 8 to 24 amino acids long. All cells throughout the body are constantly chopping up their internal proteins and displaying the resulting peptides on their surfaces. Individual cells are “interrogated” by passing T cells looking for surface peptides that are abnormal. T cells with a matching TCR have an extraordinary ability to find a rare abnormal peptide in a haystack of normal ones, and to selectively kill the cells which display that abnormal peptide.
To comprehensively find cancerous cells and cells infected by viruses, the pool of T cells in a human body includes enough distinct TCRs to recognize billions of possible antigens.
The ability of tumor cells to provoke a strong immune response is often related to the number of genetic mutations. As tumor cells proliferate, an increased frequency of mistakes in copying their DNA causes the accumulation of a variety of proteins with random substitutions, deletions, or rearrangements in their amino acid sequences. These mutant proteins generate peptides that, when displayed on the cancer cell surface, may be recognized as new antigens (neoantigens) and trigger attack by a pack of killer T cells. However, to evade attack, many potentially susceptible cancers co-opt a system of “immune checkpoints” that signal T cells to back off and not kill their targets. To overcome this problem, a class of drug called immune checkpoint inhibitors (ICIs) was developed and approved for medical use in 2011. ICIs are especially effective against tumors that accumulate many random mutations, presumably because the presence of more neoantigens can activate a larger set of killer T cells able to attack the cancer once any protective immune checkpoints are disabled.
How does this apply to fibrolamellar carcinoma (FLC)?
On the scale of mutation frequency, FLC falls at the low end of cancers, and so generates relatively few neoantigens. Perhaps for this reason, ICIs generally have not proven highly beneficial against FLC. However, a few cases of exceptionally strong clinical responses to ICIs, when given in pairs or in combination with other types of anticancer drugs, provide encouragement that highly effective immunotherapy for FLC may be achievable.
What did the St. Jude study team look for?

The six-institution study team led by Paul Thomas (St. Jude Children’s Research Hospital) and Scott Strome (University of Tennessee) explored a novel strategy towards this goal. In the published paper, they report “proof-of-concept” for a potentially universal immunotherapy for FLC, directed against a single neoantigen, the fusion protein that drives this cancer. (Allison Kirk, et al., Cell Reports Medicine, March 19, 2024)
The investigators leveraged a signature feature of FLC. As discovered by Sandy Simon (Rockefeller University) and colleagues, and reported in 2014, nearly 100% of FLC tumors arise after a loss of DNA on human chromosome 19 occurs in a liver cell, permanently joining two nearby genes to form a fused gene designated DNAJB1-PRKACA. The fusion changes and “activates” an important cellular enzyme, protein kinase A (PKA), making it cancer-causing. The gene fusion turns PKA it into a chimeric protein (abbreviated as “DP”) in which a small segment of the “PKAc” amino acid chain (the enzyme’s “catalytic subunit”) is replaced by a segment from the unrelated DNAJB1 protein. Normal PKA plays important roles in regulating cell metabolism and proliferation. However, production of the abnormal DP version of PKA, usually at elevated levels, drives the development of FLC cancers. In addition, DP remains essential for the survival and proliferation of the cancer cells as the disease progresses.
Remarkably, the joining of “D” and “P” portions of the DP chimera always occurs at precisely the same place on the two original amino acid chains. Therefore, when fragments of the cancer driving protein are displayed on the surface of FLC cells, the set of peptides spanning the junction of “D” and “P” should be unique to the cancer cells. The study team, therefore, asked if T cells that recognize DP junctional peptides can be found in FLC patients. They reasoned that such anti-DP immune cells might be enriched among “tumor-infiltrating lymphocytes” (TILS), immune cells that have migrated into tumor tissue. Furthermore, if a patient’s immune system was mounting an effective response against DP, they expected to see large numbers of T cells having TCRs specific to a junction-spanning peptide.
What did they find?
Examination of tumor samples from two dozen FLC patients did reveal the presence of TILs, although only in small numbers. About 20% of these immune cells appeared to be killer T cells. However, disappointingly, the investigators did not observe expanded clusters of killer cells bearing a selected set of TCRs, as they would have expected to see if patients were mounting very strong immune responses against their FLC cells.
Could any DP-specific killer T cells be found?
The team searched intensively for such cells in the TIL populations obtained from four additional FLC cases. From one patient, they struck gold! When they challenged this patient’s T cells with seven different overlapping peptides from the fusion junction that were predicted to be DP-specific neoantigens, a few of the patient’s T cells bound one of these peptides tightly. Furthermore, this peptide evoked a strong response from the T cells – the release of immune factors (e.g., interferon) known to be crucial in the attack of killer T cells against cancer cells. The team next isolated from these T cells the gene that encoded its unique TCR. When transferred into “naïve” T cells, this TCR gene conferred the ability to bind and respond to the correct DP junction peptide. Most importantly, the engineered T cells now recognized and killed target cells that expressed the intact DP driver protein.
Analysis of the peptide bound by the cloned TCR highlights the amazing ability of the immune system to recognize and respond to a cancer neoantigen. This peptide is 10 amino acids long. Its sequence comprises the 9 amino acids derived from the “D” protein to the left of the DP junction, plus a single adjacent amino acid from the “P” side (valine). When that “P”-derived residue was replaced with the corresponding amino acid from the normal “D” protein (glycine) the TCR’s abilities to bind the peptide and to enable killing of target cells were dramatically diminished.
How could these findings enable “precision immunotherapy” for FLC patients?
These findings point to two approaches towards immunotherapy for this cancer that are under active investigation:

- Vaccination
While it appears that few, if any, FLC patients spontaneously mount a strong immune response against the cancer’s DP driver protein, it may be possible to enhance anticancer immunity with a vaccine. Two independent research groups, one at the University of Tuebingen in Germany, another at Johns Hopkins University (Baltimore, MD), have tested this idea by vaccinating patients with a peptide corresponding to the fusion junction region of the FLC driver protein DP. Both groups used a chemically synthesized 24mer peptide, with 12 amino acids from the D and P sides of the junction.
In 2022 the Tuebingen team, led by Juliane Walz, reported encouraging results in an initial test of their anti-DP vaccine in a single FLC patient. The patient previously had suffered recurrent relapses at short time intervals after the cancer responded to chemotherapy. When the patient received the peptide vaccine, in addition to the same chemotherapy, it evoked a strong immune response. In contrast to the earlier treatments with chemotherapy alone, this time the cancer did not relapse quickly. The patient has remained apparently disease-free for more than three years. A clinical trial of that peptide vaccine (Fusion-VAC-XS15) in combination with an ICI is now underway in FLC patients (ClinicalTrials.gov ID NCT05937295).
In 2020 the Johns Hopkins group, led by Mark Yarchoan and Marina Baretti, initiated a pilot study in FLC patients of a similar peptide vaccine in combination with two ICIs (ClinicalTrials.gov ID NCT04248569). In November 2023, they reported results on the first 12 evaluable trial subjects, all who had advanced FLC. A majority of these patients (75%) developed strong immune responses to the immunizing peptide, which in most cases was associated with clinical benefit, i.e., disease stabilization or regression. Three of these patients experienced dramatic, sustained reductions in tumor burden. Two of them then had surgery to remove small areas of possible residual disease, and now appear cancer-free. The third, who did not have follow-up surgery, also currently shows no evidence of cancer. While the numbers are small, such deep, long-lasting responses in a clinical trial of a novel therapy for FLC are unprecedented.

- Cell-based immunotherapy
The Johns Hopkins and St. Jude teams have been collaborating closely in studies of immune responses against the DP fusion protein. A current shared goal is to isolate many TCR genes from patients immunized with the peptide vaccine for the fusion junction.
These anti-DP TCR genes, like the one described in the St. Jude article, could be used for precision immunotherapy by “adoptive cell therapy.” In that potential form of therapy, T cells would be taken from a patient diagnosed with FLC and genetically modified to produce a known, strong anti-DP TCR that had already been identified and cloned from an immune donor. The engineered cells would be expanded in laboratory culture and large numbers would be infused into the patient to provide an overwhelming force of T cells that are armed to hunt down and destroy FLC cancer cells. Moreover, “memory” immune cells can remain in the body throughout an individual’s lifespan. Their continuing presence could provide a perpetual defense against any surviving cancer cells that may lurk silently, only to reawaken, proliferate, and grow into recurrent tumors.
While potentially very promising, immunotherapy treatments based on TCRs have significant complexity because of how T cells recognize abnormal peptides. The peptides processed in a cell are bound into grooves of cell surface proteins of the HLA (human leukocyte antigen) system for “inspection” by surveilling T cells. Many variants of HLA proteins exist within the human population. As a result, a person’s total set of HLA proteins are a kind of genetic fingerprint, although matches of individual HLA proteins usually can be found. Immunologists have learned that a TCR that has been transferred into patient’s T cells can only recognize a peptide antigen if that peptide is displayed by a HLA protein in the new patient that exactly matches a corresponding HLA protein in the original patient. The cloned TCR the the St. Jude team described in their recent paper is based on a relatively rare HLA protein. However, it should be feasible to assemble a large enough collection of DP-specific TCRs (matched to more common HLA variants) that could enable “off the shelf” engineering of T cells for a large majority of FLC patients.
Another important area of research for immune cell-based cancer treatment is to determine whether killer T cells, identified by a marker called CD8, are indeed the most critical actors against tumors, as has been generally assumed. However, both research groups developing peptide vaccines for DP have found evidence that a different class of T cells called “helpers,” marked by CD4, play a crucial role in the immune response to the fusion protein. Efforts to isolate and characterize anti-DP TCRs from both CD8+ and CD4+ T cells are underway. This work promises to provide further insights and tools to advance immunotherapy against FLC.
What other factors influence the effectiveness of immunotherapy?
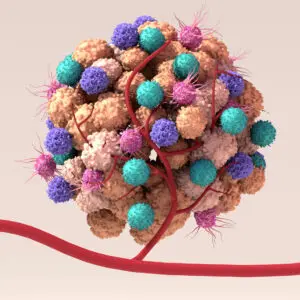
Despite remarkable progress, only a minority of cancer patients currently benefit greatly from immunotherapy. Why do tumors in some individuals appear to “melt away” upon treatment, while apparently similar tumors in others continue to progress? Many investigators point to factors in the tumor microenvironment (TME) that potentially must be overcome to make immunotherapy effective for a greater percentage of patients.
The TME is the entire “ecosystem” of a tumor, encompassing actual cancer cells, non-cancerous cells, structural proteins, nutrients, and signaling molecules. The non-cancerous components of a tumor are called the “stroma.” This includes connective tissue cells and the extracellular matrix between cells, plus blood vessels that bring in oxygen and nutrients and remove waste products. The TME also contains a variety of immune system cells, including including inflammatory cells, cells capable of specifically attacking cancer cells, and others which may suppress the anti-cancer immune response.
Deciphering the signaling systems and cellular interactions in the TME remains a major challenge in cancer research. Investigators at the University of Washington, Fred Hutchinson Cancer Center, Cornell University, St. Jude Children’s Research Hospital, and Johns Hopkins University, among others, are currently focused on defining the roles different cell types play in FLC tumor biology, and determining why T cells that target tumor-specific antigens may become dysfunctional.
What is the impact of glutamine metabolism on the immune environment?
One important feature of the TME that can strongly impact immune cells is the availability of nutrients. Proliferating cancer cells and T cells take in and use substantial quantities of glutamine, which is by far the most abundant amino acid in the human bloodstream. Recent studies indicate that FLC cells are “glutamine addicted” – that is, they depend on glutamine to support their very survival. As a FLC tumor grows and burns through glutamine, it may deplete local supplies of this essential amino acid. A deficiency of this nutrient in the TME potentially could flip anti-tumor T cells into an unresponsive state.
Furthermore, metabolism of glutamine leads FLC cells to produce lactic acid and ammonia which when released into their surroundings could further impair immune cell function. (The buildup in the bloodstream of ammonia also can lead to encephalopathy, a disturbance in brain function which is a dangerous complication in FLC patients with a high tumor burden.)
If FLC’s metabolism creates an immune suppressive tumor microenvironment, can this be corrected?
Several years ago, a team at Johns Hopkins described a new drug that potentially could both inhibit the growth of glutamine addicted cancers and restore an immune-friendly microenvironment. They began with 6-diazo-5-oxo-L-norleucine (DON), a “chemical cousin” of glutamine first tested as a potential anticancer agent in the 1950s. DON inhibits multiple enzymes that metabolize glutamine. Although DON showed some promising anti-tumor activity, it was very toxic, especially to the human gastrointestinal tract. This derailed its use as a medicine.
Recently, chemists designed a novel prodrug, DRP-104 (sirpiglenastat) that is converted into DON within tumor tissue but to an inert compound in normal tissue. In laboratory studies, the prodrug inhibited growth of glutamine-dependent tumors and also restored the function of T cells that had “shut down” in a glutamine-depleted TME. A phase 1 dose escalation/safety study of sirpiglenastat has been completed in patients with solid tumors, and this prodrug, as expected, shows much less toxicity than DON to the gut and other normal tissues.
Last year, the Yarchoan lab at Johns Hopkins tested a similar DON prodrug in combination with an ICI in mice with FLC-like liver tumors driven by the DNAJB1-PRKACA fusion gene. They observed that this regimen resulted in enhanced survival of the mice bearing the FLC-like tumors.
The identification of the glutamine addiction of FLC and the positive effects of the glutamine antagonist in mouse models led the Johns Hopkins team members to propose a new clinical trial to test the concept in FLC patients. The main goal is to test the concept that a glutamine antagonist can enhance immunotherapy in FLC patients. In addition to DRP-104, participants in the phase Ib/2 trial will receive durvalumab, an ICI that targets PD-L1. The investigators hypothesize that this combination will enable anti-tumor T cells to thrive in the tumor microenvironment, and kill FLC cells that express whatever tumor antigen(s) they may recognize. This clinical trial is currently open and is recruiting patients with advanced FLC.
Summary and implications
A therapeutic vaccine against DP given in combination with two immune checkpoint inhibitors has already induced dramatic tumor regressions in a small number of FLC patients. Additional research is necessary to extend these results and to develop immunotherapy treatments that could benefit a higher percentage of patients. Some researchers and clinicians anticipate that immunotherapy treatment regimens for FLC will eventually involve three key components:
- Vaccines or adoptive cell therapies to equip patients with large populations of specific anti-FLC T cells
- Immune checkpoint inhibitors (ICIs) to block systems that cancer cells sometimes use to evade immune attack
- Drugs to overcome other immunosuppressive features of the FLC tumor microenvironment and support a robust immune response.